Credence Bcbs Prior Authorization Form - To submit a prior authorization online, please click the button below to use the web form. In addition to this form, please fax medical records for the initial evaluation; Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member. Use the resources below to view specific drug policies and guidelines. The last five treatment notes and exercise flowsheets,. Have a specific question, or just want to talk to a real person? Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered. A prior authorization (pa) or precertification means that your plan must give prior approval before it will cover certain drugs.
The last five treatment notes and exercise flowsheets,. In addition to this form, please fax medical records for the initial evaluation; Use the resources below to view specific drug policies and guidelines. To submit a prior authorization online, please click the button below to use the web form. Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member. A prior authorization (pa) or precertification means that your plan must give prior approval before it will cover certain drugs. Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered. Have a specific question, or just want to talk to a real person?
A prior authorization (pa) or precertification means that your plan must give prior approval before it will cover certain drugs. Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member. Use the resources below to view specific drug policies and guidelines. To submit a prior authorization online, please click the button below to use the web form. Have a specific question, or just want to talk to a real person? The last five treatment notes and exercise flowsheets,. In addition to this form, please fax medical records for the initial evaluation; Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered.
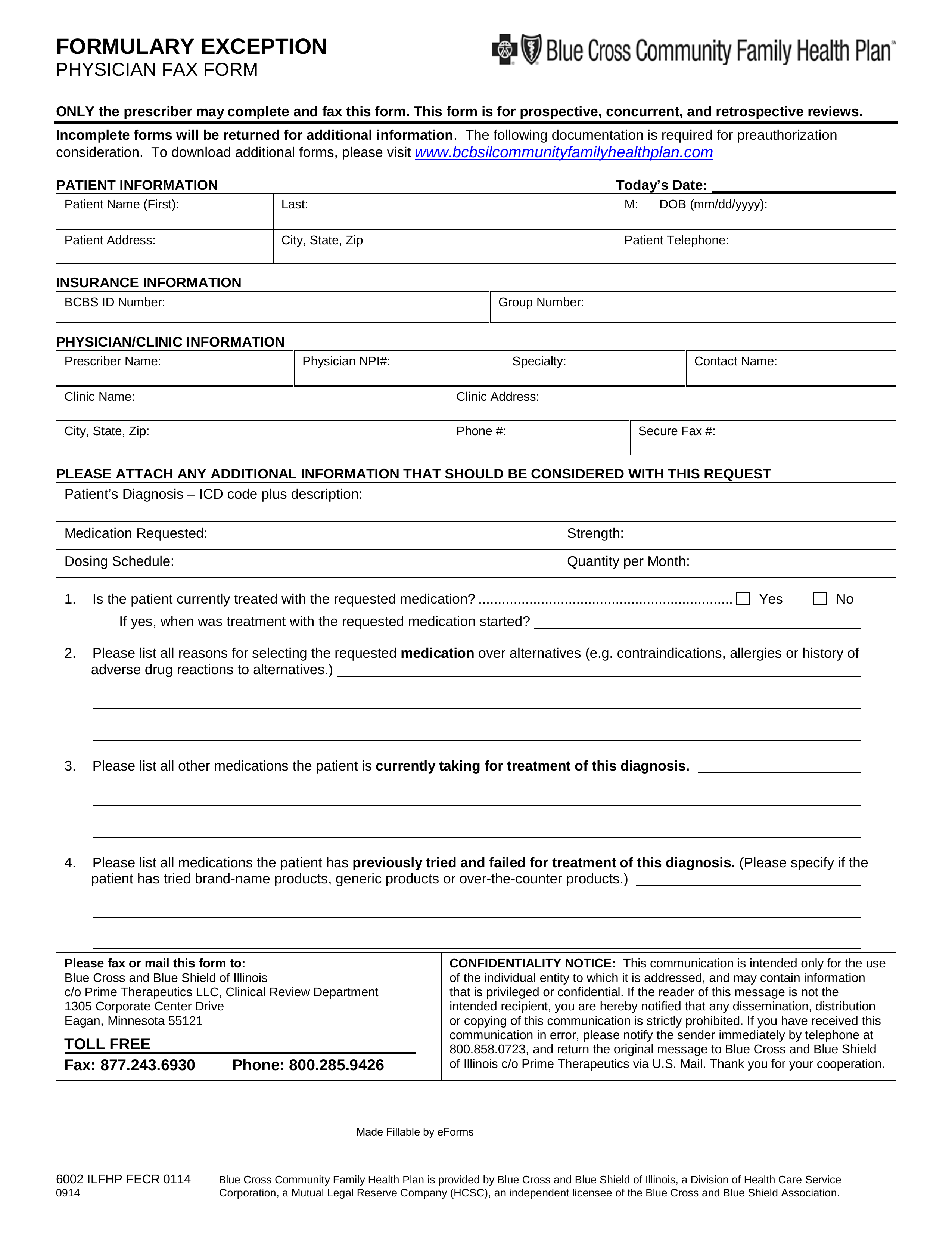
blue care network prior authorizations forms
In addition to this form, please fax medical records for the initial evaluation; Use the resources below to view specific drug policies and guidelines. To submit a prior authorization online, please click the button below to use the web form. Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member..
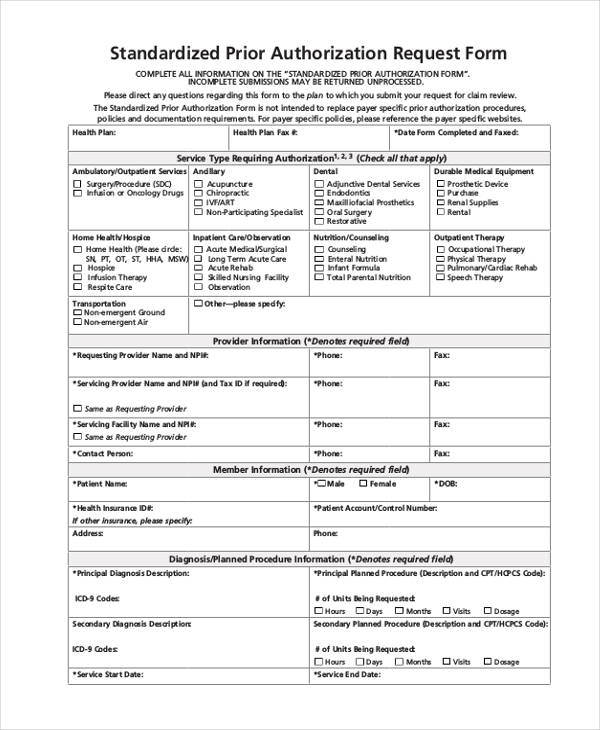
FREE 13+ Prior Authorization Forms in PDF MS Word
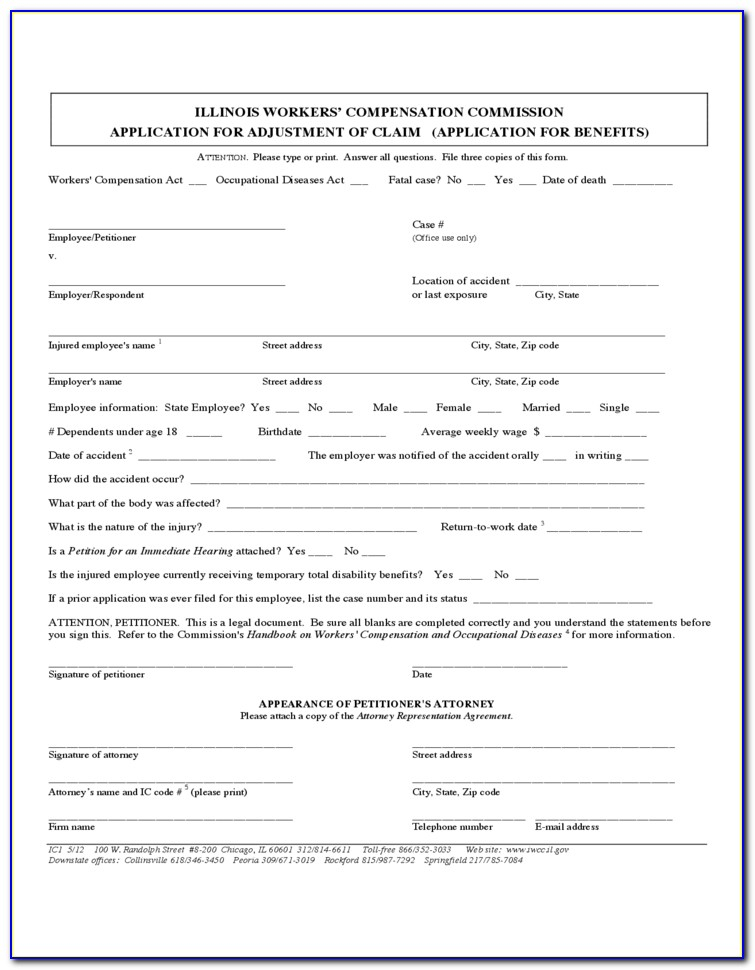
Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered. Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member. In addition to this form, please fax medical records for the initial evaluation; The last five treatment notes and exercise flowsheets,. Have a.
Blue Shield Bcbs Of Texas Prior Authorization Form
The last five treatment notes and exercise flowsheets,. Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered. A prior authorization (pa) or precertification means that your plan must give prior approval before it will cover certain drugs. To submit a prior authorization online, please click the button below to use the web.
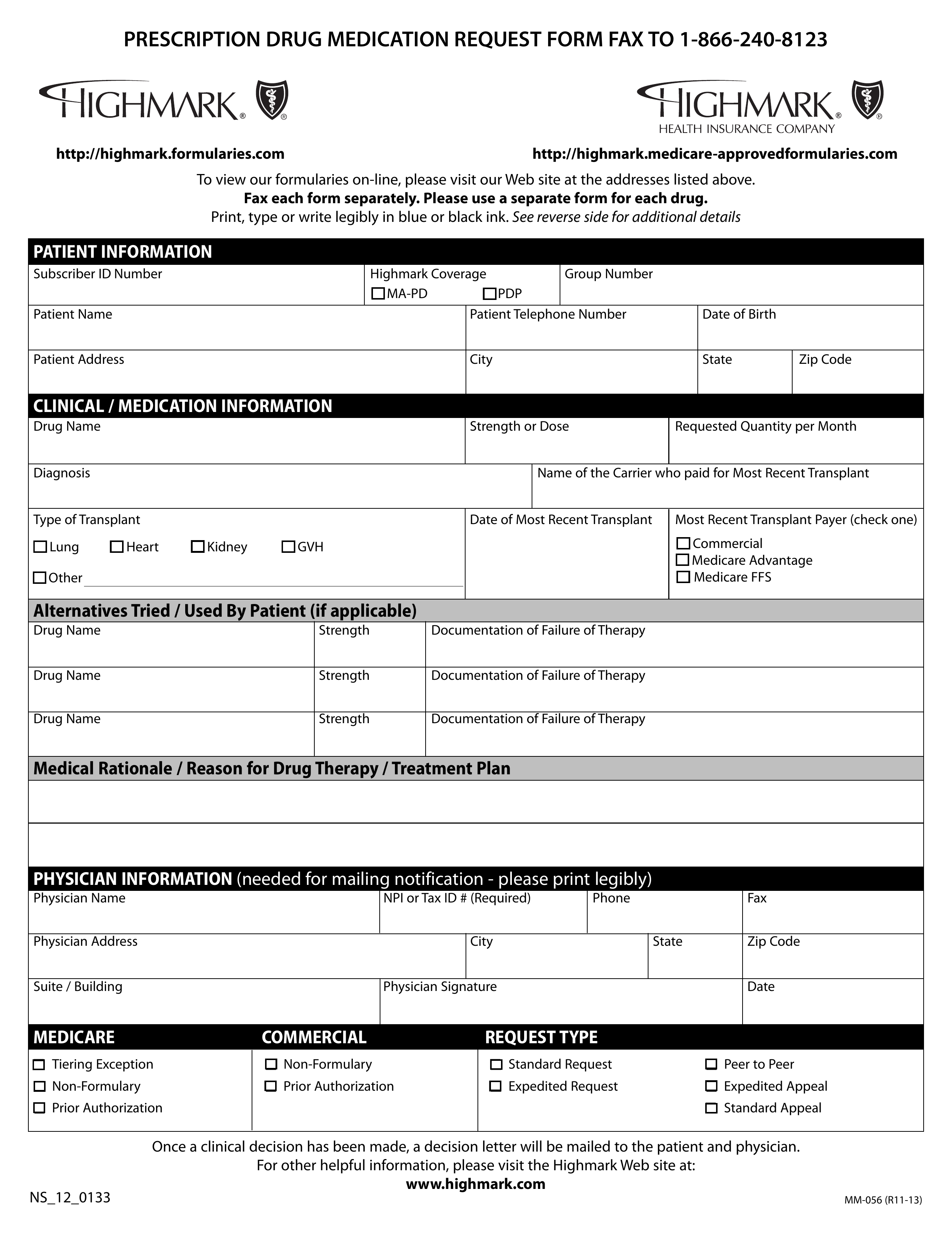
Bcbs Wegovy Prior Authorization Form
Have a specific question, or just want to talk to a real person? In addition to this form, please fax medical records for the initial evaluation; To submit a prior authorization online, please click the button below to use the web form. Use the resources below to view specific drug policies and guidelines. Always check eligibility and benefits through your.
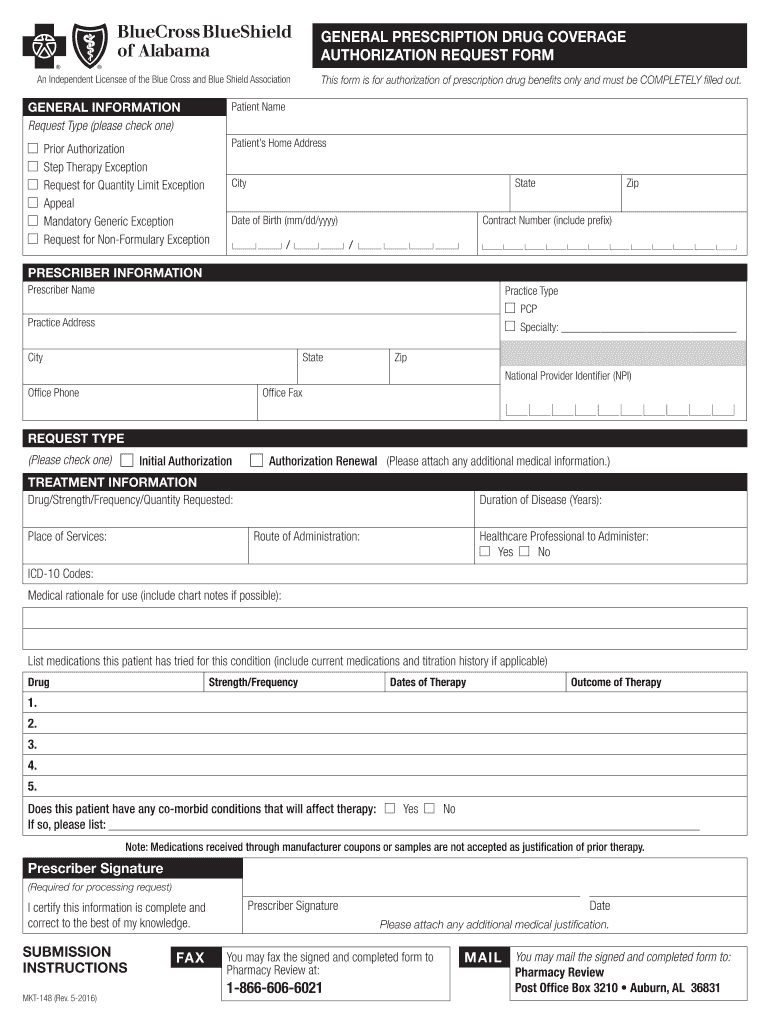
Fillable Online Bcbs Blue Advantage Prior Authorization Form Fax Email
Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered. A prior authorization (pa) or precertification means that your plan must give prior approval before it will cover certain drugs. In addition to this form, please fax medical records for the initial evaluation; Have a specific question, or just want to talk to.
Bcbs Radiology Prior Authorization Form
The last five treatment notes and exercise flowsheets,. A prior authorization (pa) or precertification means that your plan must give prior approval before it will cover certain drugs. Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member. Precertification is required for many services, including the following outpatient hospital benefits,.
Pas Alabama Com 20162024 Form Fill Out and Sign Printable PDF
The last five treatment notes and exercise flowsheets,. To submit a prior authorization online, please click the button below to use the web form. Use the resources below to view specific drug policies and guidelines. In addition to this form, please fax medical records for the initial evaluation; Have a specific question, or just want to talk to a real.
Bcbs prior auth forms to print Fill out & sign online DocHub
In addition to this form, please fax medical records for the initial evaluation; Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member. Use the resources below to view specific drug policies and guidelines. A prior authorization (pa) or precertification means that your plan must give prior approval before it.
Bcbs Prior Authorization Form Ohio Form Resume Examples 9lV8N5A30o
In addition to this form, please fax medical records for the initial evaluation; Use the resources below to view specific drug policies and guidelines. Always check eligibility and benefits through your local blue plan provider portal or your practice management system to confirm member. The last five treatment notes and exercise flowsheets,. A prior authorization (pa) or precertification means that.
Fillable Online Bcbs anthem prior authorization form for medication
A prior authorization (pa) or precertification means that your plan must give prior approval before it will cover certain drugs. The last five treatment notes and exercise flowsheets,. Use the resources below to view specific drug policies and guidelines. Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered. Have a specific question,.
A Prior Authorization (Pa) Or Precertification Means That Your Plan Must Give Prior Approval Before It Will Cover Certain Drugs.
In addition to this form, please fax medical records for the initial evaluation; Have a specific question, or just want to talk to a real person? Precertification is required for many services, including the following outpatient hospital benefits, physician benefits and other covered. The last five treatment notes and exercise flowsheets,.
Always Check Eligibility And Benefits Through Your Local Blue Plan Provider Portal Or Your Practice Management System To Confirm Member.
Use the resources below to view specific drug policies and guidelines. To submit a prior authorization online, please click the button below to use the web form.