Molina Prior Auth Form - Prior authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Obtaining authorization does not guarantee payment. Prior authorization is not a guarantee of payment for services. The plan retains the right to review benefit. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. It is needed before you can get certain services or drugs. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit limitations/exclusions.
The plan retains the right to review benefit. Obtaining authorization does not guarantee payment. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Prior authorization is not a guarantee of payment for services. It is needed before you can get certain services or drugs. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit limitations/exclusions. Prior authorization is not a guarantee of payment for services.
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Prior authorization is not a guarantee of payment for services. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Prior authorization is not a guarantee of payment for services. It is needed before you can get certain services or drugs. Obtaining authorization does not guarantee payment. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit limitations/exclusions. The plan retains the right to review benefit.
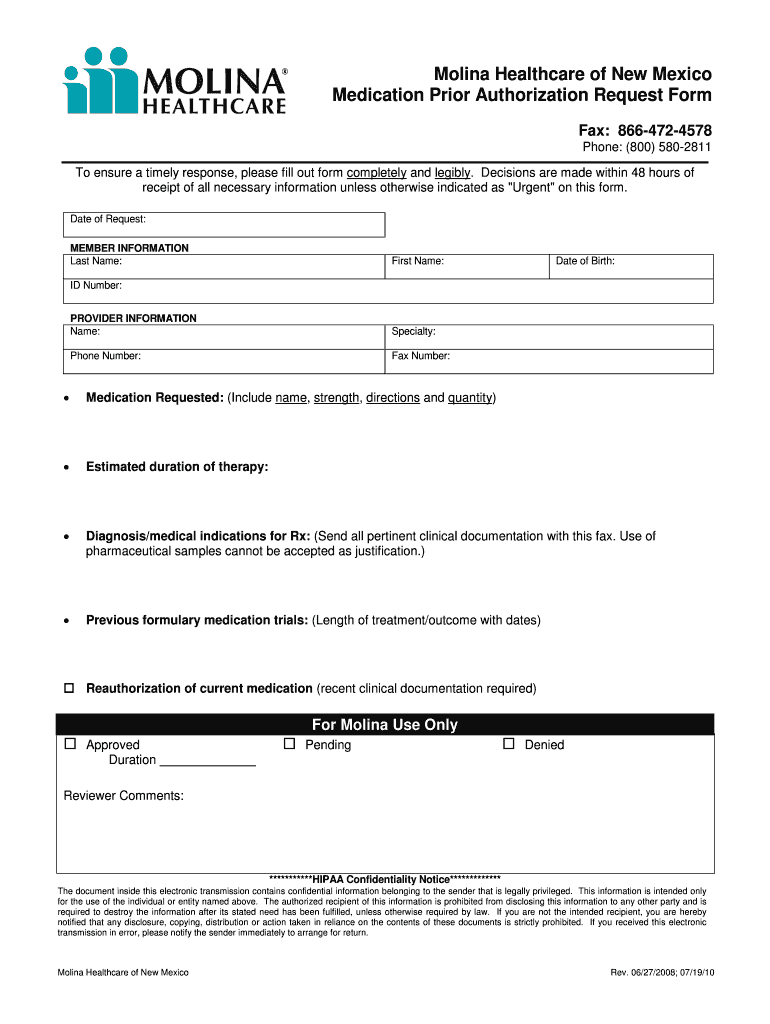
Molina Medicare Medication Prior Authorization Form Form Resume
Obtaining authorization does not guarantee payment. The plan retains the right to review benefit. Prior authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit limitations/exclusions. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
Fillable Online Molina Prior Authorization Form 2021 Fax Email Print
Obtaining authorization does not guarantee payment. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. It is needed before you can get certain services or drugs. The plan retains the right to review benefit. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
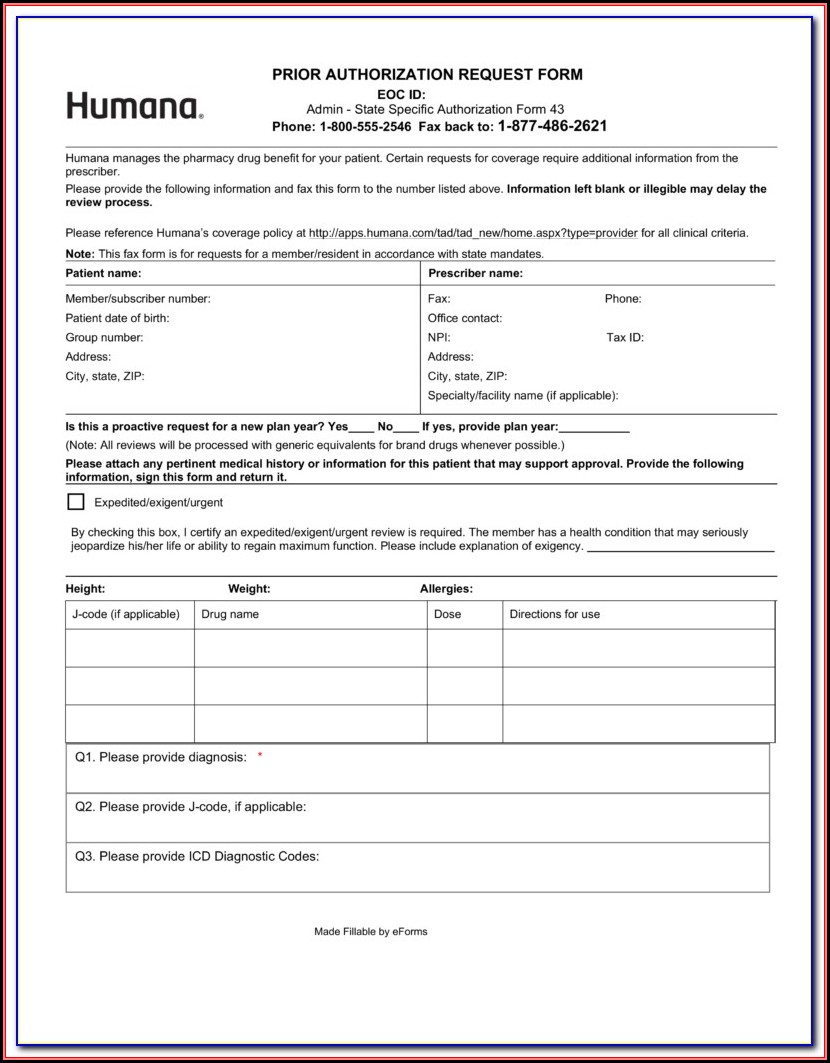
Fillable Online PDF Pharmacy Prior Authorization Request Form Molina
Prior authorization is not a guarantee of payment for services. Obtaining authorization does not guarantee payment. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. The plan retains the right to review benefit. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
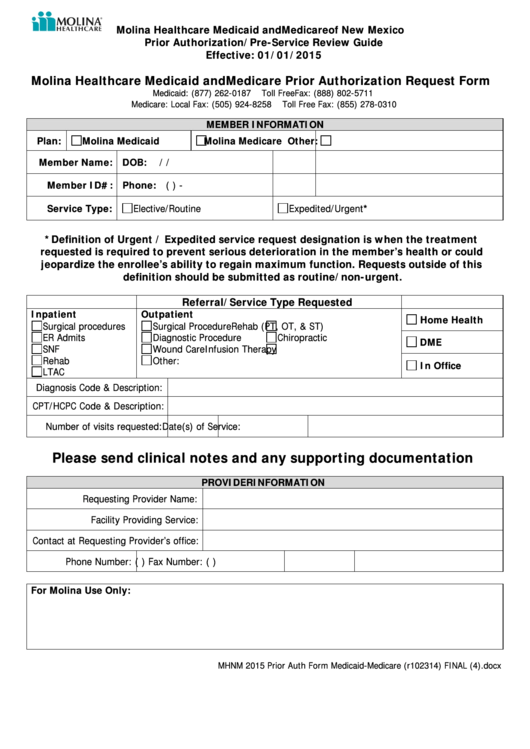
Molina Healthcare Medicaid And Medicare Prior Authorization Request
Obtaining authorization does not guarantee payment. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. It is needed before you can get certain services or drugs. The plan retains the right to review benefit. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit.
Fillable Online Molina Healthcare of Washington Prior Authorization
Prior authorization is not a guarantee of payment for services. Prior authorization is not a guarantee of payment for services. The plan retains the right to review benefit. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Obtaining authorization does not guarantee payment.
Molina Healthcare Prior Authorization Service Request Form
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Prior authorization is not a guarantee of payment for services. It is needed before you can get certain services or drugs. Obtaining authorization does not guarantee payment. Prior authorization is not a guarantee of payment for services.
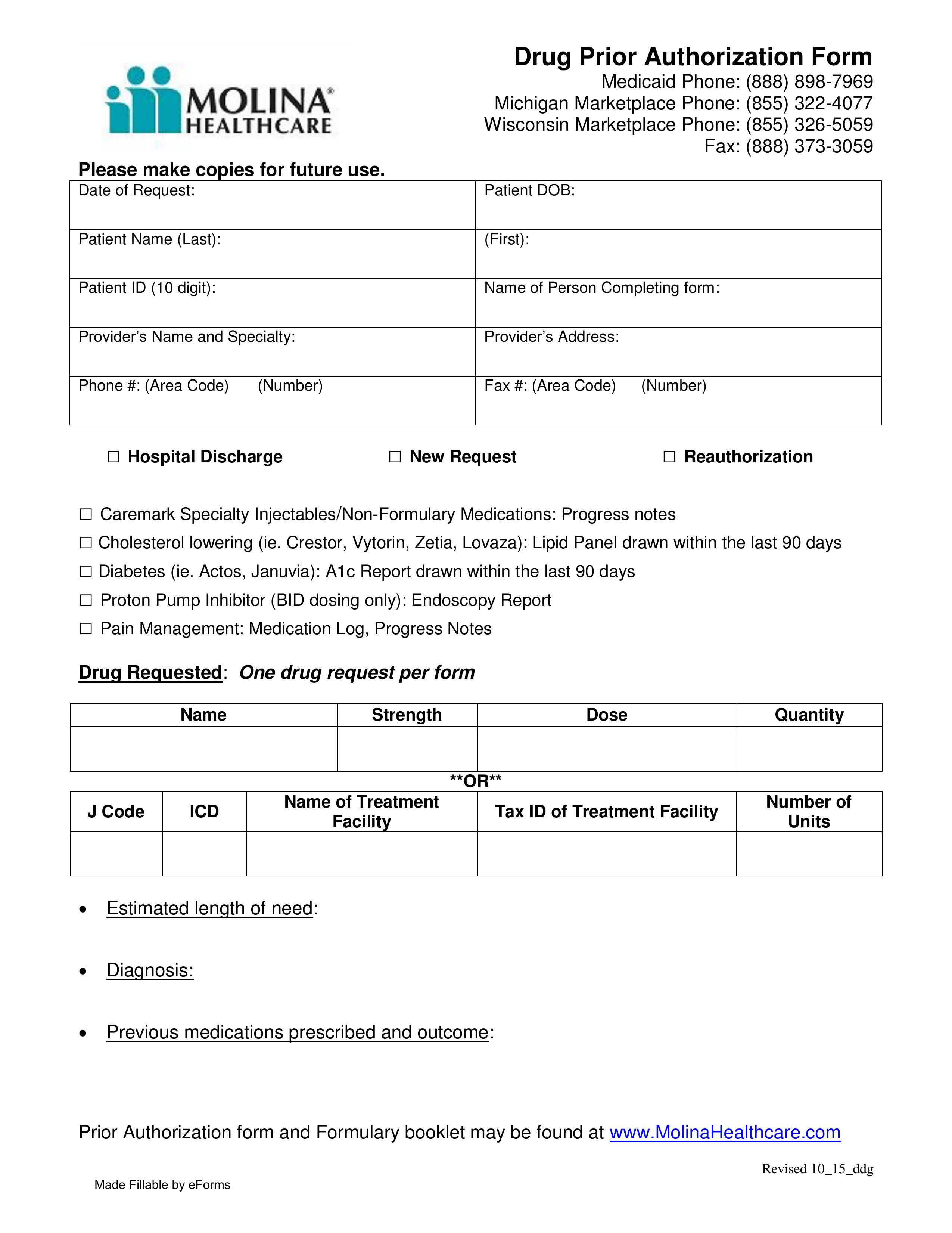
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
The plan retains the right to review benefit. It is needed before you can get certain services or drugs. Obtaining authorization does not guarantee payment. Prior authorization is not a guarantee of payment for services. Prior authorization is when your provider gets approval from molina healthcare to provide you a service.
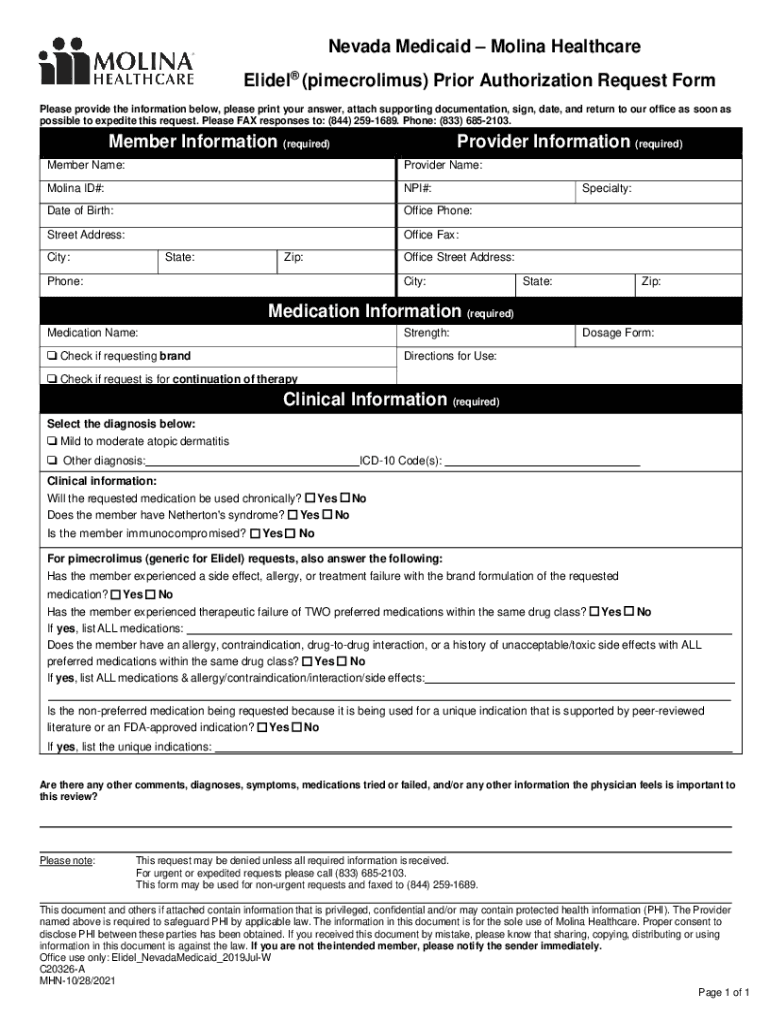
Fillable Online Medication Prior Authorization Request Form Molina
Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Prior authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. It is needed before you can get certain services or drugs. The plan retains the right to.
Molina Il Prior Auth Form Fill Online, Printable, Fillable, Blank
It is needed before you can get certain services or drugs. Obtaining authorization does not guarantee payment. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit limitations/exclusions. Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Prior authorization is not a guarantee of.
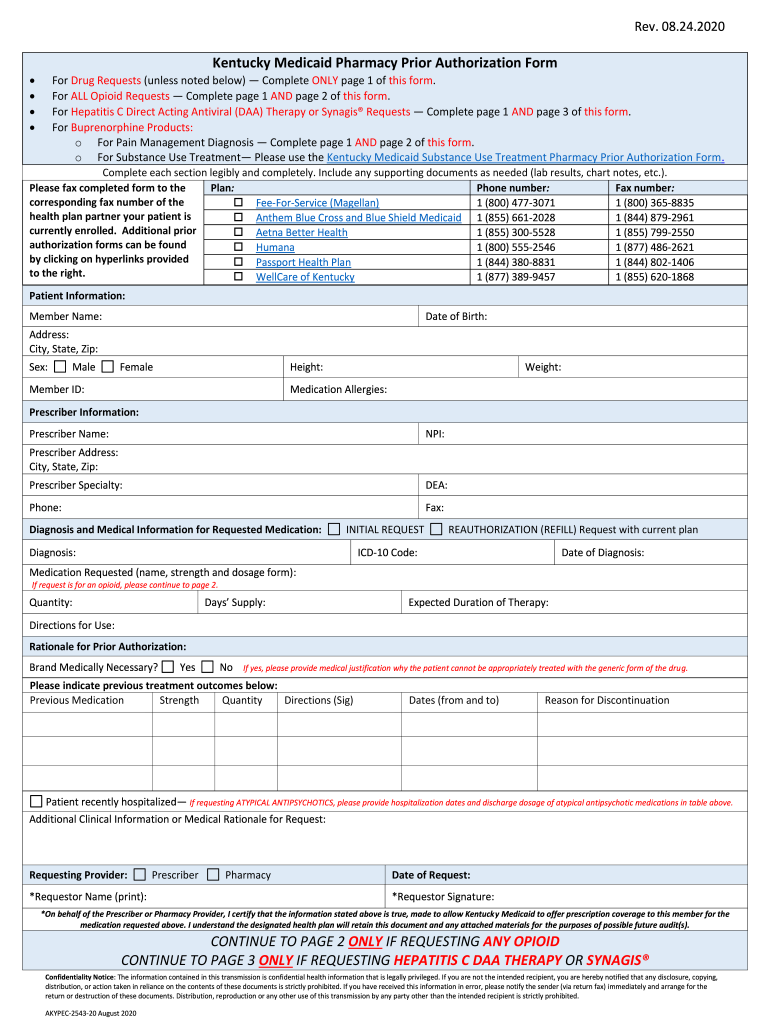
Ky medicaid prior authorization Fill out & sign online DocHub
Obtaining authorization does not guarantee payment. Prior authorization is not a guarantee of payment for services. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit limitations/exclusions. Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Prior authorization is not a guarantee of payment for.
It Is Needed Before You Can Get Certain Services Or Drugs.
Payment is made in accordance with a determination of the member’s eligibility, benefit limitation/exclusions, evidence of medical. Payment is made in accordance with a determination of the member’s eligibility on the date of service, benefit limitations/exclusions. The plan retains the right to review benefit. Prior authorization is not a guarantee of payment for services.
Obtaining Authorization Does Not Guarantee Payment.
Prior authorization is when your provider gets approval from molina healthcare to provide you a service. Prior authorization is not a guarantee of payment for services.